Biofilm-Infection Lab
About
The laboratory of implant-related infections develops and undertakes studies investigating the mechanisms of biofilm formation and attachment on biomaterial surfaces. The Biofilm-Infection Lab team has significant experience in the field of biofilm development and antimicrobial substances.
Bacterial Biofilms
By understanding the structure of biofilms and how they function we can be able to develop treatments to eliminate biofilms from implant surfaces. Biofilm in vitro models allow the testing of antimicrobial susceptibility and the analysis of biofilm architecture and molecular behaviour. In this kind of study, we investigated whether biofilms grow in vitro on metal discs and on microtiter plates. The evaluation of the biofilms formed on different surfaces is assessed by comparing the antibiotic (and other substances) susceptibility of S. aureus and by examining the structure of S. aureus biofilms grown by scanning electron microscopy (SEM). Also, several biomaterials can be tested for biofilm growth and efficacy tests for biomaterials with antimicrobial properties.
Staphylococcus epidermidis biofilm formation on metal surface (Coraça-Huber, DC)
Molecular Biology of Biofilms
A staphylococcal biofilm is produced in a two-step process: initial bacterial attachment to the surface of a foreign body or host tissue followed by a biofilm formation, consisting of bacterial proliferation, intercellular adhesion, and extracellular slime substance production. The primary attachment to a surface is related to a cell surface protein exhibiting autolysin/adhesin and fibrinogen-binding activity. This protein autolysin-E (AtlE) is encoded by the chromosomal atlE gene. Initial adhesion is mediated not only by the AtlE itself, but also via its enzymatic function. The hydrolysis of the cell wall peptidoglycan leads to autolysis and thus to the release of extracellular DNA (eDNA), which has been shown to be an important component of staphylococcal biofilms. The second stage of biofilm formation demonstrated that cell aggregation and biofilm accumulation were mediated by the products of the chromosomal ica gene locus, which is composed of four genes organized in an operon structure (icaA, icaD, icaB and icaC). The icaADBC operon leads to the production of polysaccharide intercellular adhesin (PIA) also known as poly-N-acetyl glucosamine (PNAG). Despite the undeniable important role of the icaADBC operon controlling PIA/PNAG production in staphylococcal biofilms, the existence of a PIA/PNAG-independent biofilm mechanism is known. Other important genes associated with biofilm formation and the accumulation phase in S. epidermidis are aap, fbe and embp, encoding accumulation adhesion protein (Aap), fibrinogen binding protein (Fbe) and extracellular matrix-binding protein (Embp), respectively. Embp is characterized as a giant 1MDa extracellular protein and is sufficient for biofilm formation in icaADBC- and aap-negative S. epidermidis. Potentially, as Embp and PIA can function as intercellular adhesins independently or parallel, Embp in combination with PIA can be used for development of a polyvalent S. epidermidis vaccine, for example, and improve diagnostic techniques. In the final phase of biofilm growth, cells dispersed from a mature biofilm regain the physiological characteristics of planktonic cells and may disseminate to new locations thereby causing acute infection. These biofilm-specific markers can be detected by feasible molecular methods, like polymerase chain reaction (PCR). Our objective with this research area is to better understand the pathogenesis of implant-infections and further develop new diagnostic methods for device-related infections.
Staphylococci biofilm formation steps (Coraça-Huber, DC).
Iron Chelation on the Treatment of Biofilm-Infections
The ability of certain bacteria to form biofilms underlies their capacity to cause medical device-associated infections. Most bacteria need the metal iron for their proliferation but also to form biofilms. The aim of this research area which is carried out in collaboration with Prof. Dr. Günther Weiss from the Internal Medicine MUI is to investigate whether iron restriction upon application of the iron chelator deferiprone (DFP) impacts bacterial biofilm formation and whether such an intervention can exert synergistic effects towards the antibacterial activity of three antibiotic compounds against coagulase-negative staphylococci (CNS) residing on titanium plates. In one of our studies bacteria were seeded on titanium discs and cultured to obtain biofilms. Biofilms were then exposed to DFP and/or antibiotic treatment with clindamycin, gentamycin or vancomycin. Fluorescence microscopy and scanning electron microscopy (SEM) were used for morphological analysis of the biofilms before and after treatment. Whereas DFP alone had only a moderate inhibitory effect on biofilm growth, the combination of DFP with the respective antibiotics resulted in a significant decline of bacterial numbers by two to three logs as compared to the effect of antibiotics alone. Fluorescence staining and SEM demonstrated severe damage to even complete destruction of biofilms after combined treatment with DFP and antibiotics that was not the case upon sole treatment with antibiotics. With these results we could conclude that iron chelation is able to potentiate the antibacterial activity of conventional antibiotics by destroying bacterial biofilms that recommends this combination as a promising strategy for the treatment of chronic device infections with biofilm producing CNS.
Iron chelation is able to potentiate the antibacterial activity of conventional antibiotics by destroying bacterial biofilms which recommends this combination as a promising strategy for the treatment of chronic device infections with biofilm producing CNS.
N-chlorotaurine (NCT) against Biofilms
Many orthopedic surgeons consider surgical irrigation and debridement with prosthesis retention as a treatment option for postoperative infections. Usually, saline solution with no added antimicrobial agent is used for irrigation. A remedy against biofilms resulting from surgery-related infections is highly desirable. A substance of interest is N-chlorotaurine (NCT), the main representative of long-lived oxidants produced by human granulocytes and monocytes. It can be synthesized chemically and displays broad-spectrum microbicidal properties against bacteria, viruses, fungi, and protozoa. Despite that, its oxidative reactivity is mild and its tolerability upon topical application to skin, eye and body cavities, such as the urinary bladder and joints, is high. In one of our studies in cooperation with Dr. Markus Nagl from the Department of Hygiene of the Medical University Innsbruck we found that NCT in millimolar concentrations can efficiently kill bacteria in an active and established biofilm in vitro. It seems a promising task of future studies if NCT can be used in a clinical setting to combat bacterial colonization and biofilm formation in prosthetic joint surgery as well as to fight already established infections.
XTT metabolic turnover assay. Staphylococcus aureus ATCC (left) and clinical strain (right) biofilms were incubated with 1%, 0.5% and 0.1% NCT for 15min, 30min 1h and 3h. PBS and 0.2% chlorhexidine served as negative and positive controls, respectivly. Metabolic turnover was measured by standard XTT assay (Coraça-Huber DC, et al).
Immune Responses to Biofilms
Here we study the interaction of the immune system with bacteria in nosocomial joint infections and biofilm formation. We try to create means to improve the complement mediated lysis of the bacteria. Thus, results achieved during this study not only broaden the basic knowledge about complement in nosocomial joint infections but also have clinical implications. Ultimately this induction of CML might make it possible to heal infections in vivo making graft renewal unnecessary. This study not only increases our knowledge about interactions of bacteria causing nosocomial infection with the innate immune system but can ultimately lead to the development of a novel, indirect detection strategy. This strategy could be transferred into the clinical setting adding to direct bacteriologic testing and thus helping reduce the number of false negative samples drawn from patients after joint reconstruction surgery.
|
|
On the left confocal microscopy of S. epidermidis biofilm with Life/Dead fluorescence staining (Coraça-Huber, DC, Wilflingseder, D) and on the right scanning electron microscopy of S. epidermidis biofilm (Coraça-Huber, DC).
Bone Tissue as Antibiotic Carrier
In orthopaedic surgery bone grafts are used for reconstructing bone defects caused by implant associated complications, trauma and tumors. While autografts can be used, donor site morbidity can be avoided using allografts. Bone grafts can either be used as large structural bone grafts from post-mortem donors or as bone chips from morselized femoral head donated by living patients undergoing total hip arthroplasty. Such bone chips are used to fill defects that require biomechanical stability, which can be achieved by compressing the chips into the defect site Fresh frozen bone chips are preferred because they contain the original osteoconductive and osteoinductive proteins. However, fresh frozen chips can add the risk of local contaminations. Surgery with bone allografts is complex and time-consuming; therefore it is per se prone by a higher infection rate (2.0–2.5%). Antibiotics delivered from an implanted biomaterial can be potentially used to prevent infections, providing high concentrations of antibiotics at the surgical site without local or systemic toxicity. In addition, these materials should be osteoconductive and osteoinductive, thus supporting bone healing without further surgery. Morselized bone allografts can be used as carriers by impregnating them with antibiotic solutions or by mixing them with antibiotic powders. Also, biomechanical compression tests were carried out for different preparation procedures to study the mechanical effect of grain size distribution, water and fat content and the possibility of enhancing osteoconductive and osteoinductive properties of allograft by adding bioglass or platelet rich plasma.
Morselized bone chips mixed with antibiotics and bone substitute materials (Coraça-Huber, DC et al).
Grants
MFF Tirol, Medizinischer Forschungsfond Tirol - Epitope restriction of anti - Staphylococcus antibodies in synovial fluid and serum of patients suffering from joint infection, 2017-actual.
Austrian Research Promotion Agency (FFG; Project Number: 852607) - Internship for students - Shock waves Analysis, 2015.
Coolaborators
Cornelia LASS-FLÖRL (Division of Hygiene and Medical Microbiology MUI)
Doris WILFLINGSEDER (Division of Hygiene and Medical Microbiology MUI)
Wilfried POSCH (Division of Hygiene and Medical Microbiology MUI)
Markus NAGL (Division of Hygiene and Medical Microbiology MUI)
Dorothea ORTH-HÖLLER (Division of Hygiene and Medical Microbiology MUI)
Günther WEISS (Department of Internal Medicine MUI)
Michael J. AUSSERLECHNER (Dept. of Pediatrics I; 3D Bioprinting Lab)
Marina MARCIANO (UNICAMP - FOP - Brazil)
Michel MESSORA (USP-São Paulo - Brazil)
Andrea Candido dos REIS (USP-São Paulo - Brazil)
Evandro WATANABE 8USP-São Paulo - Brazil)
Cooperation Projects
Anti-infective coating for bone allografts, within the Unit of Experimental Orthopaedics, Medical University Innsbruck, Austria (sponsored by Cells+Tissuebank Austria gem. GmbH, Austria) – 2017-actual
Efficacy of antibacterial bioactive glass S53P4 against S. aureus biofilms, within the Unit of Experimental Orthopaedics, Medical University Innsbruck, Austria (sponsored by BonAlive Biomaterials Ltd, Finland) – 2012-actual
Bone cement incorporation with antibiotics, within the Unit of Experimental Orthopaedics, Medical University Innsbruck, Austria (sponsored by Heraeus Medical GmbH, Germany) – 2015-actual
Anti-infective coatings for bone fragments, within the Unit of Experimental Orthopaedics, Medical University Innsbruck, Austria (sponsored by Telos GmbH, Germany and Heraeus Medical GmbH, Germany) – 2014-2015
Biofilm in polyvinylchloride tubing as used in dental devices, within the Unit of Experimental Orthopaedics, Medical University Innsbruck, Austria (sponsored by Metasys Medizintechnik GmbH, Austria) – 2014-2015
Anti-infective coatings, within the Unit of Experimental Orthopaedics, Medical University Innsbruck, Austria (sponsored by Heraeus Medical GmbH, Germany) – 2010-2012
Awards
2017 – Milan Biofilm Meeting 2017 – Award for the Best Poster Presentation for the study: “Iron chelation destabilizes biofilms and potentiates the antimicrobial activity of antibiotics against coagulase-negative staphylococci”.
2014 - Themistocles-Gluck-Preises from German Society of Orthopaedics and Trauma Surgery (in German: DGOOC/DGOU) for the scientific work: “Bactericidal Activity of N-Chlortaurine against Biofilm-Forming Bacteria Grown on Metal Disks”
News
Experimental Orthopedics at the 2nd International Consensus Meeting on PJI in Philadelphia 2018 ICM_biofilm.html.de
Collaboration between Innsbruck MUI and Brasilian Universities Brazil-MUI_biofilm.html.de
Publications
 |
 |
Teaching
Lab Staff
Head
|
|
Lic. Mestr. Dr. Débora Cristina Coraça-HuberSenior Scientist
Email: debora.coraca-huber@i-med.ac.atPhone: +43(0)512 9003 - 71697 |
|
|
 |
 |
 |
Employees
| |
Stephan Steixner
Research Assistant
Email: stephan.steixner@i-med.ac.atPhone:+43(0)512 9003 - 71697
|
|
|
Margot Steixner
Administration and Finances
Email: margot.steixner@i-med.ac.atPhone: +43(0)512 9003 - 71692 |
|
|
How to Find us
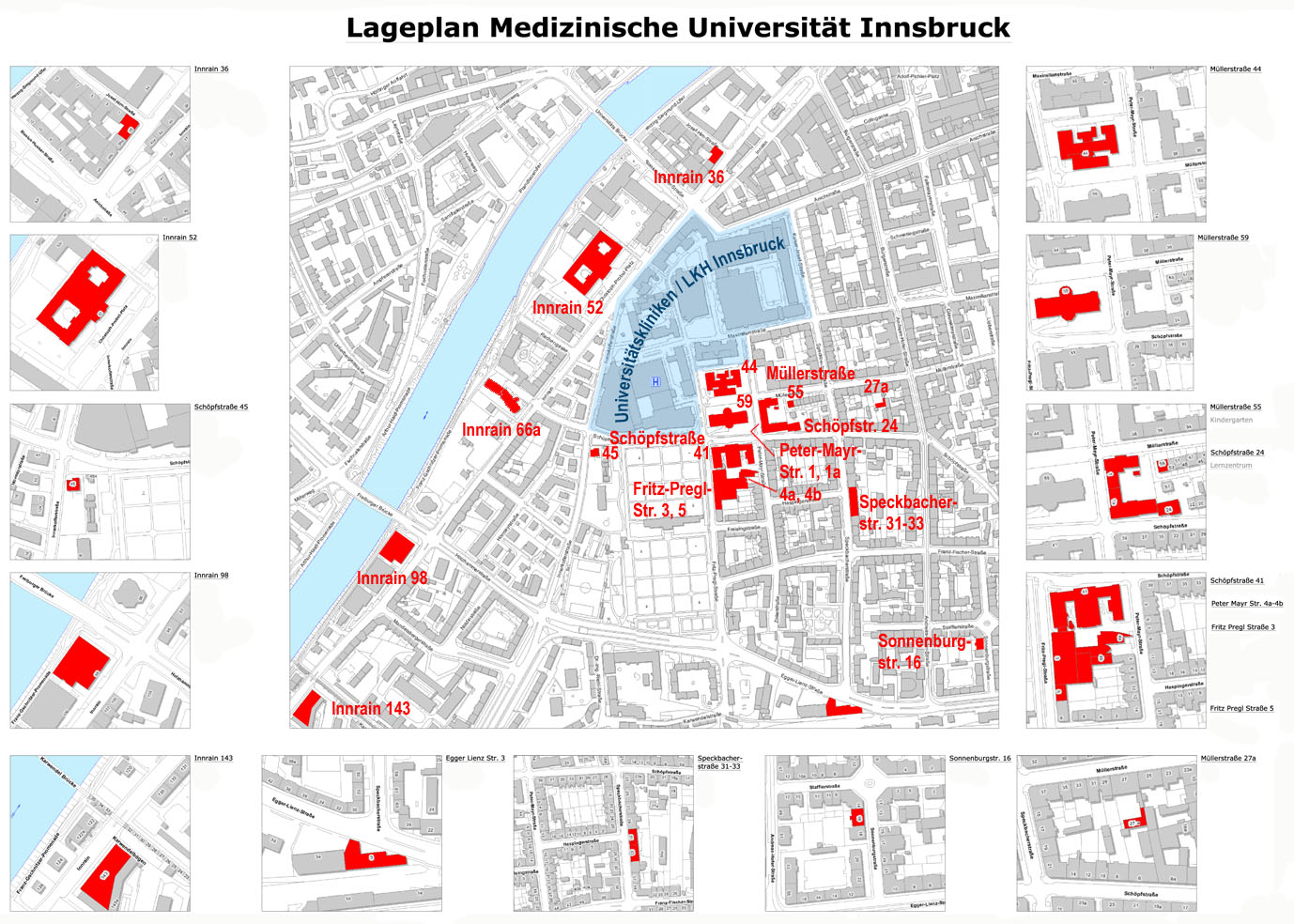
Schöpfstraße 41, UG - 6020 Innsbruck