Anaesthesia and Intensive Care
Research Focus
General Facts
Research
Selected Publications
Selected Funding, Collaboration
Devices & Services
Keywords: Anaesthesiology, critical care medicine, emergency medicine, pain medicine, palliative care, invasive ventilation, coagulation, point of care coagulation monitoring, cardiopulmonary resuscitation, perioperative medicine
Research (ÖSTAT Classification) : 301110, 301212, 301203, 301304, 301401, 301402, 301403, 302004, 302015, 302018, 302026, 302031, 302040, 302053, 302058, 302068, 302074, 302075, 302083, 302084
Research Focus
Anaesthesiology, critical care medicine, emergency medicine, pain medicine, palliative care, cardiopulmonary resuscitation, airway management, vasodilatory shock, post-traumatic shock, coagulation, hypothermia, regional anaesthesia, transplantation, neuro and obstetric anaesthesia, muscle relaxants, mountain rescue, microcirculation, prediction models, respiratory gas analysis, neuromonitoring, extracorporeal life support, ex vivo organ protection strategies, individualised ventilation, sepsis.
General Facts
The department performs about 40,000 anaesthesia cases per year, in 60 operating and diagnostic rooms. As part of a university hospital, the department covers all surgical disciplines and is responsible for six postoperative care units, three intensive care units (general surgery, trauma and transplantation critical care units), two shock rooms, the ground emergency service at two different locations (Innsbruck and Telfs), a rotor wing unit, a pain unit and an anaesthesia outpatient clinic. Because of the current Covid-19 pandemic, the department opened an additional COVID-19 ICU facility and a COVID-19 observation unit. Additionally, our physicians have teaching responsibilities (anaesthesia classes for medical students), give special skills training (first aid classes, ventilation management classes, basic life and advanced life-support training) and offer bedside teaching for our medical students during their mandatory anaesthesiology rotation. Furthermore, the Department of Anaesthesiology and Critical Care Medicine runs an experimental laboratory for basic science research and a large animal experimentation facility.
The Department of Anaesthesiology and Critical Care Medicine covers a wide variety of different activities, including all clinical aspects of anaesthesia procedures, postoperative care, intensive care medicine, emergency medicine, teaching responsibilities and various research activities.
Research
It should be noted that all anaesthesiologists involved in research activities (including basic science and clinical research) are primarily employed as physicians and clinical care providers. Only a limited part of their regular working hours is dedicated to research activities. The total amount of so-called research time for each employee varies from 10% of total working hours for a first-year resident to 40% of total working hours for a few attending physicians with certain scientific accomplishments (publications, successful grant applications, research awards). This means the Department of Anaesthesiology and Critical Care Medicine employs no full-time researchers.
However, the department is affiliated to the Institute for Respiratory Gas Analysis (Chair: Prof. Christopher Mayhew). This science research group shares a basic science laboratory with the Department of Anaesthesiology and Critical Care Medicine. There are several joint collaborations and projects with this institute.
Because of the various specialty fields and topics in anaesthesiology, researchers from the department cover many different aspects of research.
Invasive Ventilation
Patrick Spraider, Julia Abram, Gabriel Putzer, Lisa Schnegg, Judith Martini
Our group investigates flow-controlled ventilation (FCV) as a novel ventilation method established to guarantee a continuous, constant and typically identical flow during inspiration and expiration. Additionally, the constant flow coupled with direct intratracheal pressure measurement allows accurate evaluation of dynamic compliance and adjustment of ventilation settings accordingly. Our first experimental pilot study demonstrated more efficient gas exchange and improved oxygenation as well as less atelectasis in individualised FCV compared with pressure-controlled ventilation (PCV) at the best standard of care during long term ventilation. Similar results were observed in an experimental model of single lung ventilation and in an experimental model of acute respiratory distress syndrome. Two clinical ventilation studies are currently being conducted in patients undergoing cardiac surgery and thoracic surgery with single lung ventilation, comparing individualised FCV with standard-of-care PCV.
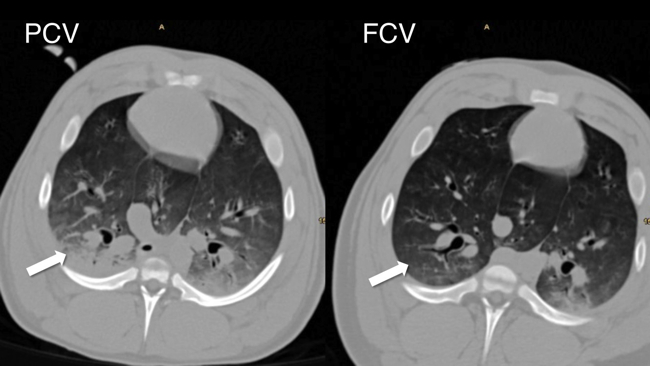
Fig. 1: Significantly reduced atelectatic lung tissue in FCV compared with PCV
Novel Organ Preservation Strategies in Transplantation Medicine
Simon Mathis, Gabriel Putzer, Martin Hermann, Lisa Schnegg, Judith Martini
A central objective of our group is to shed light on the endothelial glycocalyx and microcirculation during liver transplantation. It is already known that, during harvesting, storage on ice and subsequent reperfusion of the graft in the recipient, ischaemia reperfusion injury occurs with destruction of the glycocalyx, which is associated with poorer graft function and recipient outcome. With a new form of storage (normothermic machine perfusion), there is hope that the glycocalyx and therefore microperfusion of the graft will be better preserved. The working group is currently conducting two studies on this topic: a clinical study is investigating the effect of normothermic machine perfusion on the glycocalyx and the effects of endothelial glycocalyx shedding on perioperative organ function; an animal study is attempting to attenuate destruction of the glycocalyx through pharmacological adaptation of the perfusion solution during normothermic machine perfusion.
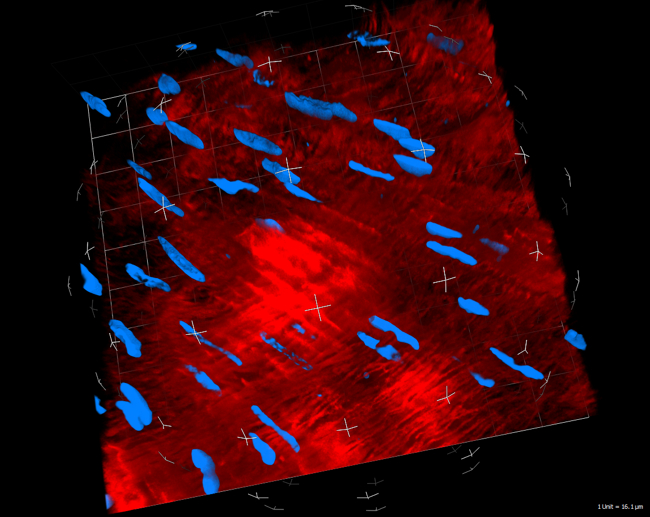
Fig. 2: Real-time, live, confocal visualisation of the glycocalyx (in red via wheat germ agglutinin) and cell nuclei (in blue via HOECHST stain). Murine blood vessel: 40x water immersion objective
Cardiopulmonary Resuscitation
Gabriel Putzer, Judith Martini, Julian Wagner, Lisa Schnegg, Peter Mair
Poor outcome after cardiac arrest is caused mainly by irreversible brain damage during cardiopulmonary resuscitation (CPR). The brain’s tolerance of hypoxia is extremely low and situations of low flow or no flow, such as during CPR, can lead to rapid progression of oxygen deficit, resulting in brain metabolic shutdown and cell death. The main research focus of this group is on investigating mechanisms that are capable of increasing oxygen availability to the brain during CPR. In particular, the effect of vasopressors on cerebral perfusion pressure and oxygen delivery to the brain have been discussed controversially in the literature. Adrenalin, which has been used during CPR for decades, has been accused of diminishing microvascular perfusion, owing to strong vasoconstriction, which leads to poor oxygenation of downstream tissues. Recent results of this research group challenge this hypothesis by using a complex neuromonitoring model in pigs, which includes not only oxygenation parameters but also direct microvascular perfusion measurements and metabolic profiles.
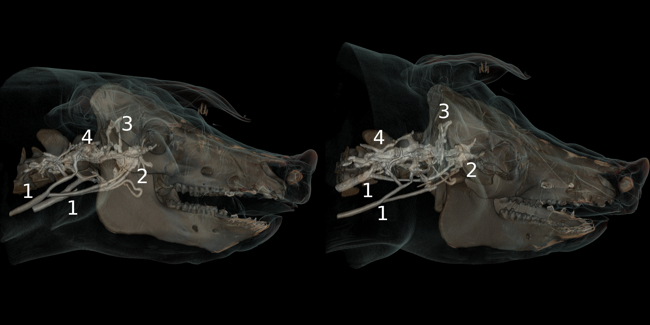
Fig. 3: Angiographic preliminary study of porcine cerebral venous drainage
Coagulopathy in Critically Ill Patients
Dietmar Fries, Mirjam Bachler, Benjamin Treichl, Volker Schäfer, Johannes Bösch, Benedikt Treml
Our focus is on the crosstalk between inflammation and coagulation in critically ill patients. Endothelial damage as a result of inflammatory processes causes a strong pro-coagulatory shift in haemostasis, which is associated with increased morbidity and mortality. We were able to prove that critically ill COVID-19 patients suffer from severe hypercoagulability as a result of fibrinolytic shutdown and heparin resistance. The phenomenon of heparin resistance was described first in our post-surgical, trauma and sepsis patients and later in critically ill patients suffering from COVID-19, who were treated in our institution. Alternative treatment strategies for anticoagulation of these particular patient groups were established in our institution.
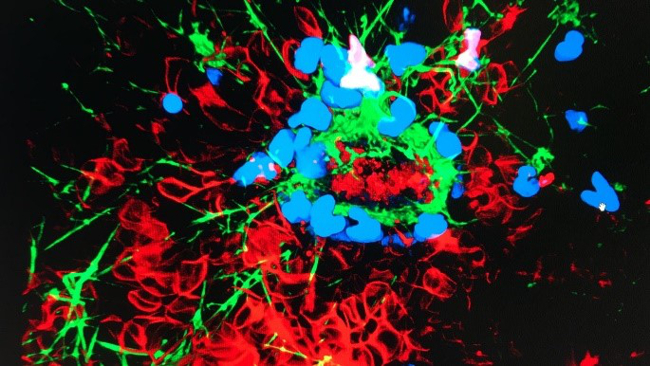
Fig. 4: NETosis = neutrophil extracellular traps in a COVID-19 patient with fibrin deposits (green) and signs of coagulation activation
Emergency and Alpine Medicine
Dietmar Fries, Mirjam Bachler, Mathias Ströhle, Benedikt Treml, Janett Kreutziger
Pre-hospital emergency care, especially in our Alpine region, is a further field of interest. Our department initiated, coordinated and completed an international, multicentre trial in bleeding trauma patients. Subsequently, members of our research groups also examined pre-hospital airway management.
Organ Dysfunction in Critically Ill Patients
Dietmar Fries, Mirjam Bachler, Anna Brandtner, Benedikt Treml, Christopher Rugg
The investigation and treatment of renal dysfunction is another focus of our ICUs. Our department was involved in a multinational, multicentre clinical trial with the aim of identifying the best timing for initiation of renal replacement therapy. The results of this study were published in 2020 in the New England Journal of Medicine.
Another focus of our department is on haemostatic derangements caused by hepatic dysfunction. Here in particular, the balance between bleeding and thrombosis is very complex. A current project is investigating new coagulation parameters, including the effect of fibrinogen concentrate on coagulation in patients with advanced liver disease.
A historical field of research in our department is the treatment of oxygenation and ventilation disorders in critically ill patients on mechanical ventilation. As part of a basic science project in collaboration with the Department of Physiology and EURAC, Bolzano, a new method for faster measurement of the oxygen-binding curve was established under various conditions and patented. The consequences of normobaric hypoxia and the consequences of extracorporeal blood purification on the use of catecholamines and survival in critically ill patients are being examined in the context of other projects.
Institute of Breath Gas Analysis
Christopher Mayhew, Vera Ruzsanyi
The main research focus of this group is on the detection of volatile components of breath by proton-transfer reaction – time of flight – mass spectrometer (PTR-ToF-MS, Ionicon Analytik GmbH) and the use of a gas chromatograph – ion mobility spectrometer (GC-IMS, University of Hannover). Current studies include:
- In vitro studies of volatile components of bacteria or different cell lines;
- Detection of human volatile components of breath or urine after natural disasters (e.g. earthquakes);
- Anaesthesiological respiratory monitoring after surgical procedures.
Pre-Hospital Emergency Medicine, Quality and Risk Management
Michael Baubin, Agnes Neumayr
Key topics of our research group focus on the improvement of medical care as well as risk and quality management in pre-hospital emergency medicine. One main objective, for example, is the continuous development of a benchmark report on a regional and international level, including comparison of the quality of the Tyrolian emergency services e.g. with those in Bavaria and Baden-Württemberg, Germany. As the physician-staffed EMS Innsbruck participates in the German cardiopulmonary resuscitation registry – GRR – we use this international database for research studies, in order to analyse and improve the treatment of out-of-hospital cardiac arrest in multiple aspects. Another current research project is focusing on the assessment of critical incidents and never events in ambulance services, in order to develop an S2 guideline for risk management in pre-hospital emergency medicine together with research partners from Germany and Switzerland.
Selected Publications
Invasive Ventilation
- Spraider, P.; Martini, J.; Abram, J.; Putzer, G.; Glodny, B.; Hell, T.; Barnes, T.; Enk, D.: Individualized flow-controlled ventilation compared to best clinical practice pressure-controlled ventilation: a prospective randomized porcine study. CRITICAL CARE. 2020; 24(1): 662.
- Enk, D.; Spraider, P.; Abram, J.; Barnes, T.: Pressure Measurements in Flow-Controlled Ventilation. CIRTICAL CARE MEDICINE. 2020; 48(12): e1359-e1360.
Novel Organ Preservation Strategies in Transplantation Medicine
- Putzer, G.; Martini, J.; Gasteiger, L.; Mathis, S.; Breitkopf, R.; Hell, T.; van Enckevort, A.; Oberhuber, R.; Öfner, D.; Schneeberger, S.: Liver Transplantation Activity in the Eurotransplant Area Is Recovering Slowly During the COVID-19 Crisis. TRANSPLANTATION DIRECT. 2020; 6(11): e611.
- Cardini, B.; Oberhuber, R.; Fodor, M.; Hautz, T.; Margreiter, C.; Resch, T.; Scheidl, S.; Maglione, M.; Bösmüller, C.; Mair, H.; Frank, M.; Augustin, F.; Griesmacher, A.; Schennach, H.; Martini, J.; Breitkopf, R.; Eschertzhuber, S.; Pajk, W.; Obwegeser, A.; Tilg, H.; Watson, C.; Öfner, D.; Weissenbacher, A.; Schneeberger, S.: Clinical Implementation of Prolonged Liver Preservation and Monitoring Through Normothermic Machine Perfusion in Liver Transplantation. TRANSPLANTATION. 2020; 104(9): 1917-1928.
Cardiopulmonary Resuscitation
- Putzer, G.; Martini. J.; Spraider, P.; Hornung, R.; Pinggera, D.; Abram, J.; Altaner, N.; Hell, T.; Glodny, B.; Helbok, R.; Mair, P.: Effects of different adrenaline doses on cerebral oxygenation and cerebral metabolism during cardiopulmonary resuscitation in pigs. RESUSCITATION. 2020; 156: 223-229
- Schiefecker, A.J.; Putzer, G.; Braun, P.; Martini, J.; Strapazzon, G.; Antunes, A.P.; Mulino, M.; Pinggera, D.; Glodny, B.; Brugger, H.; Paal. P.; Mair, P.; Pfausler, B.; Beer, R.; Humpel, C.; Helbok, R.: Total Tau-Protein as Investigated by Cerebral Microdialysis Increases in Hypothermic Cardiac Arrest: A Pig Study. THERAPEUTIC HYPOTHERMIA AND TEMPERATURE MANAGEMENT. 2020; online ahead of print
- Gaasch, M.; Putzer, G.; Schiefecker, A.J.; Martini, J.; Strapazzon, G.; Ianosi, B.; Thome, C.; Paal, P.; Brugger, H.; Mair, P.; Helbok, R.: Cerebral Autoregulation Is Impaired During Deep Hypothermia-A Porcine Multimodal Neuromonitoring Study. THERAPEUTIC HYPOTHERMIA AND TEMPERATURE MANAGEMENT. 2020; 10(2): 122-127
Coagulopathy in Critically Ill Patients
- Bachler, M.; Bösch, J.; Stürzel, D.P.; Hell, T.; Giebl, A.; Ströhle, M.; Klein, S.J.; Schäfer, V.; Lehner, G.F.; Joannidis, M.; Thomé, C.; Fries, D.: Impaired fibrinolysis in critically ill COVID-19 patients. BRITISH JOURNAL OF ANAESTHESIA. 2020; 126(3): 590-598
- Bachler, M.; Hell. T.; Bösch, J.; Treml, B.; Schenk, B.; Treichl, B.; Friesenecker, B.; Lorenz, I.; Stengg, D.; Hruby, S.; Wallner, B.; Oswald, E.; Ströhle, M.; Niederwanger, C.; Irsara, C.; Fries, D.: A Prospective Pilot Trial to Assess the Efficacy of Argatroban (Argatra®) in Critically Ill Patients with Heparin Resistance. JOURNAL OF CLINICAL MEDICINE. 2020; 9(4): 963
- Brandtner, A.; Bachler, M.; Fries, D.; Hermann, M.; Ruehlicke, J.; Fux, V.; Griesmacher, A.; Niederwanger, C.; Hell, T.; Treml, B.: Tigecycline Interferes with Fibrinogen Polymerization Independent of Peripheral Interactions with the Coagulation System. ANTIBIOTICS (BASEL). 2020; 9(2): 84.
Emergency and Alpine Medicine
- Ziegler, B.; Bachler, M.; Haberfellner, H.; Niederwanger, C.; Innerhofer, P.; Hell, T.; Kaufmann, M.; Maegele, M.; Martinowitz, U.; Nebl, C.; Oswald, E.; Schöchl, H.; Schenk, B.; Thaler, M.; Treichl, B.; Voelckel, W.; Zykova, I.; Wimmer, C.; Fries, D.: Efficacy of prehospital administration of fibrinogen concentrate in trauma patients bleeding or presumed to bleed (FIinTIC): A multicentre, double-blind, placebo-controlled, randomised pilot study.
EUROPEAN JOURNAL OF ANAESTHESIOLOGY. 2020; online ahead of print. - Walsh, M.; Thomas, S.; Kwaan, H.; Aversa, J.; Anderson, S.; Sundararajan, R.; Zimmer, D.; Bunch, C.; Stillson, J.; Draxler, D.; Balogh, Z.J.; Fries, D.: Modern methods for monitoring hemorrhagic resuscitation in the United States: Why the delay? JOURNAL OF TRAUMA AND ACUTE CARE SURGERY. 2020; 89(6): 1018-1022.
- Mitteregger, T.; Schwaiger, P.; Kreutziger, J.; Schöchl, H.; Oberladstätter, D.; Trimmel, H.; Voelckel, W.G.: Computer tomographic assessment of gastric volume in major trauma patients: impact of pre-hospital airway management on gastric air. SCANDINAVIAN JOURNAL OF TRAUMA, RESUSCITATION AND EMERGENCY. 2020; 28(1): 72.
Organ Dysfunction in Critically Ill Patients
- STARRT-AKI Investigators*; Canadian Critical Care Trials Group; Australian and New Zealand Intensive Care Society Clinical Trials Group; United Kingdom Critical Care Research Group; Canadian Nephrology Trials Network; Irish Critical Care Trials Group; Bagshaw, S.M.; Wald, R.; Adhikari, N.K.J; Bellomo, R.; da Costa, B.R.; Dreyfuss, D.; Du, B.; Gallagher, M.P.; Gaudry, S.; Hoste, E.A.; Lamontagne, F.; Joannidis, M.; Landoni, G.; Liu, K.D.; McAuley, D.F.; McGuinness, S.P.; Neyra, J.A.; Nichol, A.D.; Ostermann, M.; Palevsky, P.M.; Pettilä, V.; Quenot, J.P.; Qiu, H.; Rochwerg, B.; Schneider, A.G.; Smith, O.M.; Thomé, F.; Thorpe, K.E.; Vaara, S.; Weir, M.; Wang, A.Y.; Young, P.; Zarbock, A.: Timing of Initiation of Renal-Replacement Therapy in Acute Kidney Injury. THE NEW ENGLAND YOURNAL OF MEDICINE. 2020; 383(3): 240-51. * Fries Dietmar and Bachler Mirjam
- Rugg, C.; Ströhle, M.; Treml, B.; Bachler, M.; Schmid, S.; Kreutziger, J.: ICU-Acquired Hypernatremia Is Associated with Persistent Inflammation, Immunosuppression and Catabolism Syndrome. JOURNAL OF CLINICAL MEDICINE. 2020; 9(9): 3017.
- Rugg, C.; Klose, R.; Hornung, R.; Innerhofer, N.; Bachler, M.; Schmid, S.; Fries, D.; Ströhle, M.: Hemoadsorption with CytoSorb in Septic Shock Reduces Catecholamine Requirements and In-Hospital Mortality: A Single-Center Retrospective 'Genetic' Matched Analysis. BIOMEDICINES. 2020; 8(12); 539.
Breath Gas Analysis
- Malásková, M.; Olivenza-León, D.; Chellayah, P.D.; Martini, J.; Lederer, W.; Ruzsanyi, V.; Unterkofler, K.; Mochalski, P.; Märk, T.D.; Watts, P.; Mayhew, C.A.: Studies pertaining to the monitoring of volatile halogenated anaesthetics in breath by proton transfer reaction mass spectrometry. JOURNAL OF BREATH RESEARCH. 2020; 14(2): 026004
Pre-Hospital Emergency Medicine, Quality and Risk Management
- Krebs, S.; Roth, D.; Knoflach, M.; Baubin, M.; Lang, W.; Beisteiner, R.; Purrucker, J.; Poli, S.; Sykora, M.: Design and derivation of the Austrian Prehospital Stroke Scale (APSS) to predict severe stroke with large vessel occlusion. PREHOSPITAL EMERGENCY CARE. 2020; 17: 1-8
- Gräsner, J.T.; Wnent, J.; Herlitz, J.; Perkins, G.D.; Lefering, R.; Tjelmeland, I.; Koster, R.W.; Masterson, S.; Rossell-Ortiz, F.; Maurer, H.; Böttiger, B.W.; Moertl, M.; Mols, P.; Alihodžić, H.; Hadžibegović, I.; Ioannides, M.; Truhlář, A.; Wissenberg, M.; Salo, A.; Escutnaire, J.; Nikolaou, N.; Nagy, E.; Jonsson, B.S.; Wright, P.; Semeraro, F.; Clarens, C.; Beesems, S.; Cebula, G.; Correia, V.H.; Cimpoesu, D.; Raffay, V.; Trenkler, S.; Markota, A.; Strömsöe, A.; Burkart, R.; Booth, S.; Bossaert, L.: Survival after out-of-hospital cardiac arrest in Europe - Results of the EuReCa TWO study. RESUSCITATION. 2020; 148: 218-226
- Golger, P.; Karl, A.; Unterlechner, W.; Schinnerl, A.; Baubin, M.; Neumayr, A.: Risiko „Belassung“: Ein Perspektivenwechsel. RETTUNGSDIENST. 2020; (8), 20-24
Selection of Funding
Collaborations
- University of California - Department of Bioengineering, San Diego, USA
- University Hospital of Münster – Dietmar Enk, P, MD, Münster, Germany
- University of Greenwich – Tom Barnes, MSc, PhD, London, United Kingdom
- U.S. Army Institute of Surgical Research – Dr. Wenjun Martini, San Antonio, USA
- EURAC Research – Department of Physiology, Bolzano, Italy
- Austrian Association for Alpine and High-altitude Medicine (ÖGAHM), Mieming, Austria
- MHS Medical School Hamburg – Prof. Dr. Dr. Rainer Petzina / Dr. med. Hartwig Marung, Hamburg, Germany
- Institut für Notfallmedizin und Medizinmanagement – INM, LMU Klinikum – Dr. med Bert Urban / Dr. med. Marc Lazarovici, Munich, Germany
- Rettung Basel-Stadt – Dr. med. Marc Lüthy, Basel, Switzerland
- Ministry of Defence and Sports (Bundesministerium für Landesverteidigung und Sport), Austria
Devices & Services
- Large animal experimental facility
- Confocal microscope laboratory
- General research laboratory
 o.Univ.-Prof. Dr. med. univ. Karl Lindner
o.Univ.-Prof. Dr. med. univ. Karl Lindner
Director
Contact:
Anichstraße 35
6020 Innsbruck
Austria
Email:karl.lindner@i-med.ac.at
Phone: +43 512 504 28505
Fax: +43 512 504 28507
https://anaesthesia.tirol-kliniken.at



